Consider getting your baby an Apple iPad. The iPad is a perfect toy for your baby because as she is playing with it, she is learning from it. And as she grows, it can grow with her into a diverse learning and communication tool.
Five Favorite Apps for Baby
 Sound Shaker by Tickle Tap Apps 1.99 - touted as the 21st century rattle, Sound Shaker lets children create and play with chime, whistle, drum, barnyard animal and mystery sounds by simply tapping and tilting. Repeated taps generate new sounds, while longer taps grow sounds and trigger surprise animations. Tilting makes sounds spin and collide in whimsical combinations.
Sound Shaker by Tickle Tap Apps 1.99 - touted as the 21st century rattle, Sound Shaker lets children create and play with chime, whistle, drum, barnyard animal and mystery sounds by simply tapping and tilting. Repeated taps generate new sounds, while longer taps grow sounds and trigger surprise animations. Tilting makes sounds spin and collide in whimsical combinations.  Itsy Bitsy Spider by Duck Duck Moose 1.99 - A musical book based on the popular song, with fully interactive, original illustrations. Follow the spider through the captivating, inter-connected scenes as he goes up the water spout, comes down with the rain, and watches the sun dry up all the rain.
Itsy Bitsy Spider by Duck Duck Moose 1.99 - A musical book based on the popular song, with fully interactive, original illustrations. Follow the spider through the captivating, inter-connected scenes as he goes up the water spout, comes down with the rain, and watches the sun dry up all the rain.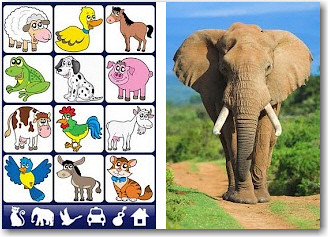 Sound Touch by Sound Touch 3.99 - Sound Touch has 6 categories, which are shown at the bottom of the screen as pictures – animals, wild animals, wild birds, vehicles, musical-instruments and household. Each page has 12 items displayed with bright, cute cartoon items. Tap a picture, and a real life photo of the item pops open, accompanied by the sound it makes. Tap the picture anywhere, and it disappears. There is a sound option in settings that makes it so that the app says the name of the item prior to making the sound.
Sound Touch by Sound Touch 3.99 - Sound Touch has 6 categories, which are shown at the bottom of the screen as pictures – animals, wild animals, wild birds, vehicles, musical-instruments and household. Each page has 12 items displayed with bright, cute cartoon items. Tap a picture, and a real life photo of the item pops open, accompanied by the sound it makes. Tap the picture anywhere, and it disappears. There is a sound option in settings that makes it so that the app says the name of the item prior to making the sound. Peekaboo Barn By Night & Day Studios, Inc. 1.99 - This cute app features barnyard animals and the sounds they make. Babies can open the barn doors to find a new animal animation by touching the screen. They’ll learn about cause and effect and become familiar with animal names and sounds. As a bonus, you can record your own voice saying the animal name.
Peekaboo Barn By Night & Day Studios, Inc. 1.99 - This cute app features barnyard animals and the sounds they make. Babies can open the barn doors to find a new animal animation by touching the screen. They’ll learn about cause and effect and become familiar with animal names and sounds. As a bonus, you can record your own voice saying the animal name. Talking Tom Cat By Out Fit 7 Ltd. Free- Baby’s first pet :-) Tom the cat responds to your touch and repeats everything you say or babble with a funny voice. When you pet him, he purrs.
Talking Tom Cat By Out Fit 7 Ltd. Free- Baby’s first pet :-) Tom the cat responds to your touch and repeats everything you say or babble with a funny voice. When you pet him, he purrs.Ok, stop. Yes, I know an iPad is a really expensive toy for a one-year-old, but consider it an investment. New iPads start at $500, and first generation iPads can be found on auction sites and lists for about $200-ish. Here are some ideas on how you might afford an iPad for your baby with Down syndrome.
Chip-in birthday gift: Perhaps for your baby’s first birthday you could create a chip-in fund and let family and friends know that you are trying to raise enough for an iPad for your little one.
Medicaid Coordinator Alternative Funding: If your child has Medicaid or the Medicaid Waiver, your coordinator may be able to find you grant funding for your baby’s iPad.
Win one: iPads are a popular draw for online fundraisers. Keep your eye out for the chance to win one. Usually you can get a drawing entry by donating a small amount or even just by posting the fundraiser on your FB, blog, or Twitter account. Right now through March 31st, Patti over at A Perfect Lily is giving away a beautiful brand new iPad 3 as part of a very special adoption fundraiser, so be sure to head over there and get an entry to win.
Update: Two more chances to win an iPad... (valid to 4/6/12) over at Our Chinese Butterfly and (valid to 4/8/12) over at The Stars Aligned.
Babyproofing the iPad
If you do get an iPad for your little sweetie, be sure to babyproof it with a back shell
Your Turn
Do you already have an iPad for your child with Ds? What are your favorite apps?